Dr. Stephen Pistorius is a Senior Research Scientist at CancerCare Manitoba and the Research Institute in Oncology and Hematology, the Director of the Medical Physics Graduate Program, a Professor of Physics & Astronomy and an Associate Professor of Radiology at the University of Manitoba.
According to Breastcancer.org, 12% of women in developed countries will develop invasive breast cancer at some point in their lifetime.
This means that one in eight women will be affected by breast cancer.
The incidence of breast cancer in low-and-middle-income countries (LMIC) is lower than in the wealthier nations, but the mortality rates are higher. For example, the American Cancer Society report on Cancer in Africa (2011) states that “the five-year survival rate for breast cancer is less than 50% in Gambia, Uganda, and Algeria, compared to nearly 90% in the United States.” Similar disparities in cancer mortality are also found between rural and urban centers in developed countries.
Early detection of breast cancer has a direct impact on the survival rates of women. While X-Ray mammography is the standard for breast cancer imaging, it has some limitations. These include:
- The use of x-rays that are a form of ionising radiation, which can cause cancer
- The need for breast compression, which may be uncomfortable for the woman
- The relatively high cost that limits the availability of mammography in low-income countries
- The need for trained personnel to operate the system and to interpret the images
With support from Grand Challenges Canada, which is funded by the government of Canada, we at the University of Manitoba are evaluating the feasibility of a portable breast microwave sensing system which aims to improve the availability of breast cancer pre-screening in low- and middle-income countries and in rural communities in developed nations – a potential example of reverse innovation.
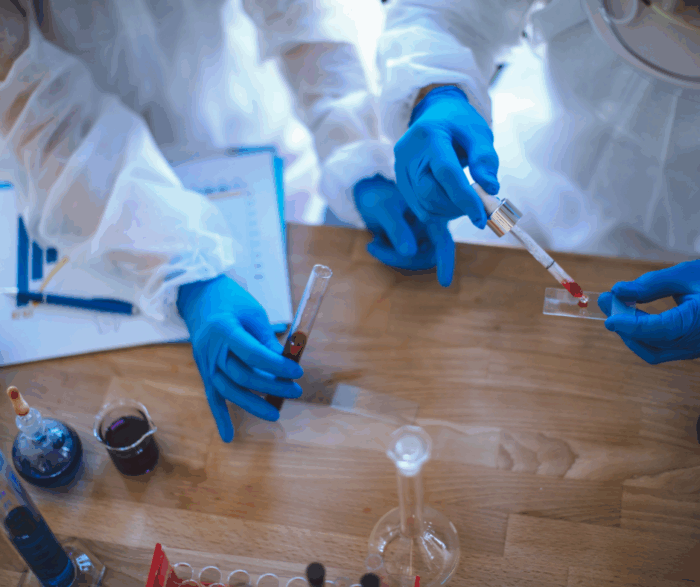
Microwave signals similar to those used by commercial cellphones can be directed towards a breast, where they will scatter when they interact with different types of tissue. Breast tumours scatter more than normal tissues and a group led by Professor Stephen Pistorius at the University of Manitoba is using these physical phenomena to come up with alternative methods of detecting the presence of a tumour in the breast.

An inexpensive, suitcase-sized system has been designed and built using technologies similar to those found in mobile phones. (Fig 1) These include radio-frequency (wireless) instrumentation, compact antennas and specially designed solid-state sensors. Embedded system technology is used to provide the computational power needed to carry out the data collection, to classify the results and to interface with the client in a comprehensive but non-verbal way (Fig 2). The data collection is quick, taking less than one minute per breast, while the expert system, which identifies whether a tumour is present, takes only another minute to process the results. If a response from the breast indicates that a tumour may be present, the woman is directed to a health care professional for further evaluation and testing.

Good progress is being made on both technical and business fronts, and a four-person team of MBA students were very successful in a recent pitch day competition, where the idea and system design won the top student award, the people’s choice award and where they took the second place overall. The business case envisages being able to distribute the system in Manitoba in 2018 with further expansion into other Canadian provinces and into Africa in the following year.
The feedback from our volunteers in Africa (Fig 3) who were involved in our usability study, and from participants in a survey of health care practitioners has been positive, and we are continuing to test, adapt and improve the design and the classification algorithms of the system. Interestingly, while one-third of the participants indicated some level of concern about the use of microwaves, almost 100% of the volunteers felt that they would use the system at least once a year, and 90% of the participants felt that they could operate the system by themselves.

Further testing of the system and communication about the safety and benefits of the system, needs to be carried out if it is to become suitable for widespread use. The process has not been without its challenges, and we have realised that obtaining the necessary regulatory approvals will be more challenging than initially envisaged.
While the excitement of developing and testing the device cannot be downplayed, the most rewarding part of this project to date has been to experience the excitement and involvement of the volunteers in Africa. The participation was amazing and with the help of our academic partners in Abuja (Nigeria) and Cape Town (South Africa), we were able to obtain valuable input into how the system can and should be improved. The participation of non-governmental agencies was instrumental in enabling us to interact with as many people as we did, and we are looking forward to returning to both of these regions in 2016 to evaluate the system further.
Our research team is broadening its base and has also established research partnerships with the National University of Galway (Ireland) and at Oxford University (UK) to help advance this project. The development of this device, which has potential benefits for women across the world, would not have been possible without the financial support of Grand Challenges Canada, CancerCare Manitoba and the University of Manitoba. The dedication of the students and collaborators at the University of Manitoba, the University of Cape Town, the National Hospital in Abuja, and Project Pink Blue – Health and Psychological Trust Centre in Nigeria is also gratefully acknowledged.
Learn more about this project on their project page on the Grand Challenges Canada website.
We encourage you to post your questions and comments about this blog post on our Facebook page Grand Challenges Canada and on Twitter @gchallenges.