Tesfalem Teshome (MSc) is a Lecturer of Public Health and Researcher at Hawassa College of Health Sciences in Hawassa, Ethiopia, and is the project lead of the Stars in Global Health Project “Acceptability, feasibility and viral, nutritional, immunologic and microbiologic safety of flash-heated treatment of breast milk: preventing postnatal transmission of HIV through modifying breast-feeding practices in developing countries.”
World Breast Feeding week (August 1 to 7) is an important reminder about breast milk’s distinct and irreplaceable value to the human infant, and an opportunity to advocate the importance of breast feeding for better health and the healthy development of infants.

Breastfeeding provides numerous short and long-term benefits for both mother and child (win-win approach). These include a solid foundation for lifetime cardiovascular health, greater resistance to childhood infectious diseases, enhanced immunity, improved cognitive functions, and reduced risk chronic diseases, such as diabetes. Breast milk has all the nutrients babies need to stay healthy and grow. It requires no mixing, sterilization or equipment. It is always at the right temperature and environmentally friendly. Breastfeeding can also help mothers with child spacing and reduce their risk of cardiovascular disease, breast and ovarian cancer, type 2 diabetes and post-partum depression. It is economical for families, employers, healthcare systems and nations as a whole as it preserves valuable resources, including money, time, safe water and fuel. Virtually all children benefit from breast-feeding, regardless of where they live.
According to WHO, the optimal feeding pattern for overall child survival is exclusive breast-feeding for the first 6 months and continued breast-feeding for up to 2 years and beyond, with complementary feeding from the age of 6 months.
Sadly, HIV-infected mothers may transmit the virus to their infants through breast feeding. For HIV-infected mothers in the developed world, avoidance of breast-feeding is recommended. However, for mothers in developing countries, a similar recommendation may not be a safe due to factors including but not limited to the cost of infant formula, lack of safe water, unsanitary living conditions and socio-cultural situations. In these settings, formula feeding has been associated with a 14 to 25 fold increase in diarrhea-associated infant mortality because of contamination and lack of the protective factors intrinsic to breast milk.
After weighing the risk of Mother To Child Transmission Of HIV/AIDS associated with breast feeding against the possibility of greater dangers posed by infant formula, it appears that HIV-infected mothers in the developing countries should exclusively breastfeed their infants for the first 6 months of life, introducing appropriate complementary foods thereafter, and continue breast feeding for the first 12 months of life. In these cases, both the mother and her infant should take antiretroviral drugs for Prevention of Mother To Child Transmission Of HIV/AIDS.
This is something challenging in Ethiopian context, where about only 24% of HIV-infected pregnant women and 19% of HIV-exposed children were receiving antiretroviral drugs. As a result HIV-exposed infants are at increased risk of acquiring HIV during the course of breast-feeding. So, it is clear that there should be some alternative to make breast milk safer for infants born to HIV-infected mothers in such contexts.
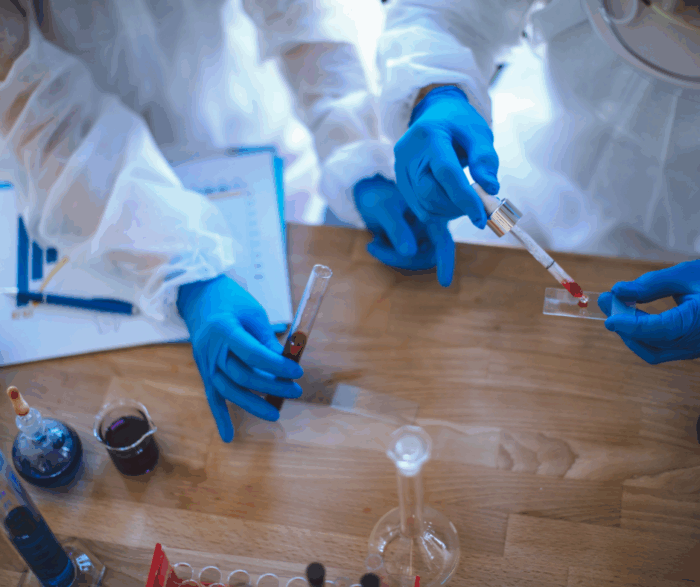
Through the support of Grand Challenges Canada, which is funded by the Government of Canada, our team has been conducting a pilot intervention-study with Hawassa College of Health Sciences to test the acceptability and sustainability of a flash-heating treatment of breast milk for infants in the Southern part of Ethiopia. Flash heating is a simple in-home breast milk pasteurization method which mothers in developing countries can implement over an outdoor fire or in the kitchen using ordinary equipment that can be found in simple homes. Based on Grand Challenges Canada’s vision for integrated innovation, our project has an integrated nature involving societal, business and scientific components.
We selected seven midwives to recruit HIV-infected pregnant women for the study and three Health Officers to undertake Clinical, Nutritional and Developmental follow up for infants. We also hired eight Research Nurses to conduct home based follow up for infants and one supervisor. After three days of intensive training, HIV-infected pregnant women were counselled and recruited. Then, they were categorized into either the flash heat-treated breast milk or standard breast feeding group based on their infant feeding choice. Research Nurses have been closely following all the infants from right after delivery up until six months of age through regular home visit. Focus group discussion and in-depth interview with key informants were used to investigate issues related to the acceptability and sustainability of the method.
Currently we are in the last phase of the project, in which Research Nurses are conducting a home based follow up. A preliminary result from focus group discussions indicates that mothers using Flash heat treated breast milk feel that this procedure is reducing their concerns about their infant contracting the virus, even if the procedure somewhat requires the support of fathers and other family members.
We thank Dr. Mesfin Beyero, Mr. Kare Chawicha, Mr. Wosenyeleh Semeon and the dedicated research team for their commitment to this project.
We encourage you to post your questions and comments about this blog post on our Facebook page Grand Challenges Canada and on Twitter @gchallenges.